The Modern guide to ovulation predictor kits and ovulation tests

Reviewed by Nataki Douglas, MD, PhD,
Written by Talia Shirazi, PhD
last updated: Jun 03, 2022
13 min read
Here's what we'll cover
When it comes to uterus owners trying to conceive, doctors and “Dr. Google” may advise you to track your cycle to help you better time intercourse. After all, there’s only a brief window (called the “fertile window”) when conception is actually possible. If you're not trying to conceive, cycle tracking can also help you simply learn more about your menstrual cycle — before or after stopping hormonal birth control.
While there are many different methods used to track your cycle, this post will focus on one of the most tried-and-true, science-backed methods we’ve got: ovulation predictor kits, also called OPKs or ovulation tests. An ovulation test (like Modern Fertility’s Ovulation Test) is a home test that harnesses what we know about hormonal changes during your cycle to determine if you’re in your fertile window.
Find answers to these questions here:
What is an ovulation test?
An ovulation test, aka an ovulation test kit or OPK, is a urine test that measures the levels of luteinizing hormone (LH) in your body, a hormone that peaks before ovulation to signal to your maturing follicle that it’s time to release an egg. Here are some of the most important things to know about OPKs:
Some tests tell you whether your LH is above or below a certain threshold. These are called threshold-based tests. These will give you a positive result or negative result. Problem is, the average ovulation test doesn't work for about 1 in 10 of us. Threshold-based tests are designed around averages of what an LH surge “should” look like, but bodies are all different. At least 1 in 10 women surge at a level that typically isn’t detected by these binary positive/negative tests. People with low LH levels can end up seeing “negative” all the time… even if they are ovulating.
Other tests, like Modern Fertility’s Ovulation Test, will actually quantify your LH levels for you. These are called semi-quantitative tests. They give you a numerical value of your LH, telling you where it falls within a range. We might be biased, but we love semi-quantitative tests, since they can give you a better idea of how your LH is changing over time, help you understand LH patterns, and can pinpoint your most fertile days — meaning the days when you have the highest chances of getting pregnant.
Some ovulation tests do the interpretation for you (digital tests), and others don’t (analog tests). There’s a little more user error in interpreting analog tests.
In general, most ovulation tests are accurate for most people. However, if you have atypically high or low LH, if you don’t have a typical LH surge (or if you have two!), or if you have a hormone-related condition (like PCOS), not all ovulation tests will catch ovulation. In these cases, semi-quantitative tests may work better — but it’ll all depend on your hormones.
How do ovulation tests work? What’s the basic science they rely on?
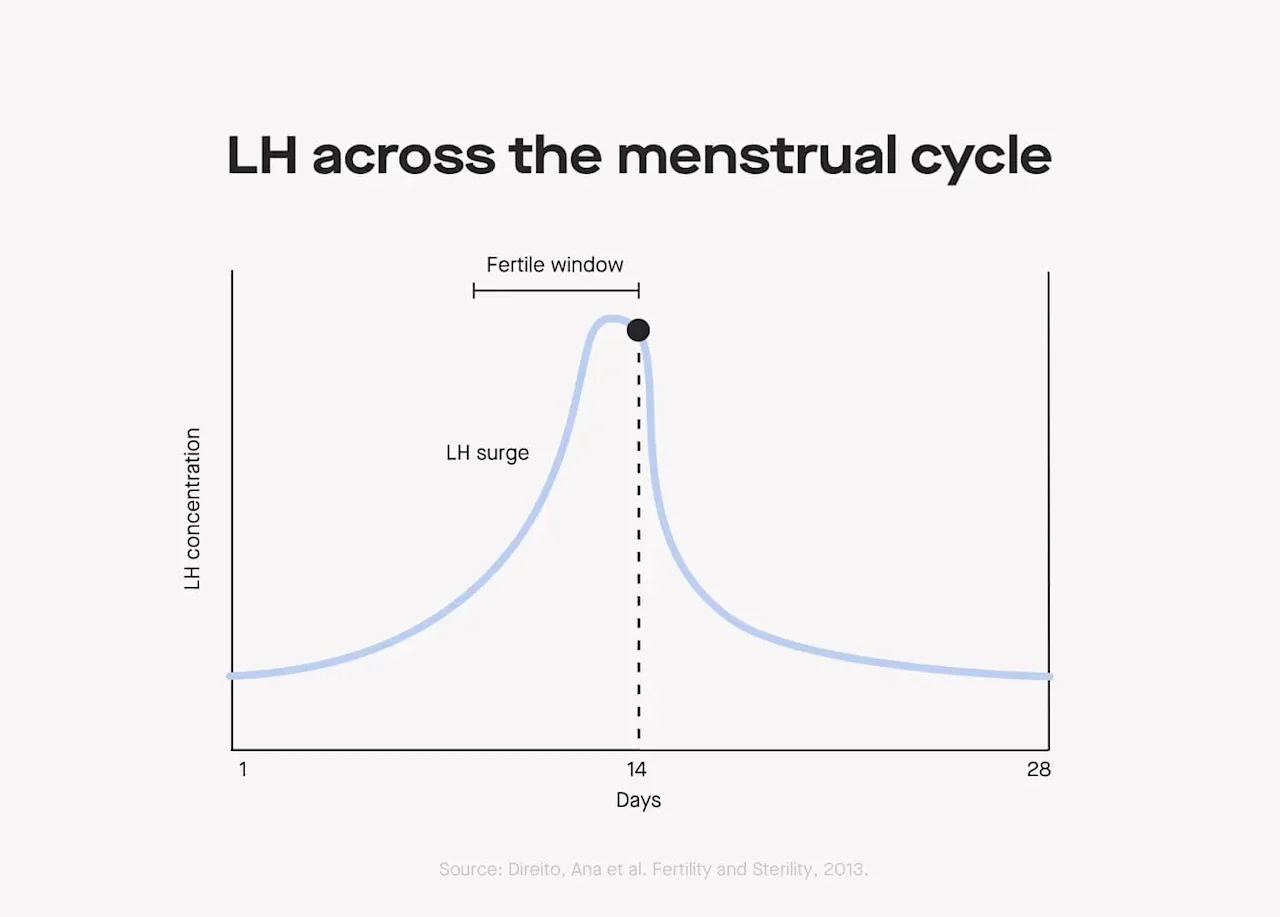
The logic behind ovulation tests is based on hormonal shifts across natural menstrual cycles — more specifically, they’re based on peaks in luteinizing hormone (LH) that happen before ovulation.
(Note: If you are on hormonal birth control like the pill or the implant, or have certain conditions like polycystic ovary syndrome (PCOS), these patterns might not apply to you — more on that in a bit.)
Here’s what’s happening in your body during ovulation:
At the onset of your period, your body has low levels of important reproductive hormones, such as LH, follicle-stimulating hormone (FSH), and estradiol (E2).
In the two-ish weeks after your period starts, the dominant follicle develops. It contains the egg that will eventually get released — and the follicle produces more and more E2 as it develops.
Around , there are large surges of LH and FSH which will trigger the follicle to release an egg (read: ovulation).
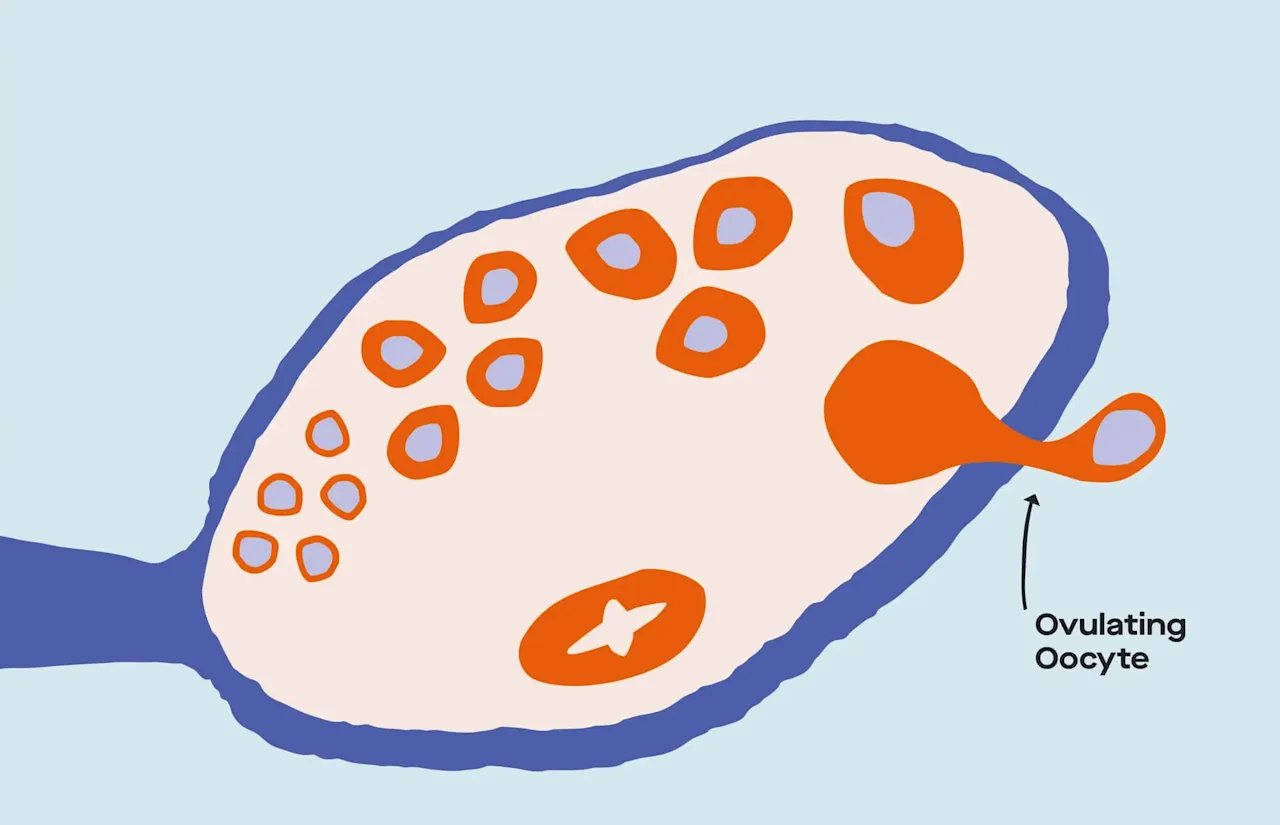
LH surges are necessary for ovulation: If there’s an LH surge, chances are pretty darn high that ovulation is coming right up. If there’s sperm hanging around once the egg has been released into the fallopian tubes, conception is possible (though not guaranteed).
But, a quick disclaimer
What we described is the pattern of hormonal changes across a cycle that you’d see in any reproductive endocrinology textbook or med school curriculum. It’s true that for most people with ovaries, for most cycles, this is the general pattern that’s followed.
But it’s possible for this pattern to look different in different people, and for this pattern to look different across cycles for the same person. As we mentioned above, the average threshold-based ovulation test doesn't work for about 1 in 10 of us who don't surge at a level that's typically detected by binary positive/negative tests.
Another example: Though we typically describe ovulatory cycles as having one very short LH surge, it’s also possible to have two LH surges, or even a single “plateau” that’s characterized by a prolonged period of high LH. Recent studies using detailed hormone measurements across cycles highlight the amount of variability in what cycles look like and challenge our previously held understanding of what we should be considered “normal.”
If you have a condition like PCOS that impacts reproductive hormones, it’s possible that you don’t ovulate frequently, and thus wouldn’t exhibit the patterns described in the last section. The same applies for those on some types of hormonal birth control, like combined oral contraceptives, which specifically work to inhibit ovulation by suppressing LH and FSH, among other processes.
What are the different types of ovulation tests?
Ovulation testing overwhelmingly relies on measuring levels of LH in your urine to estimate whether you may be ovulating (and thus at peak fertility). Some ovulation tests will also measure E2, which can help you to better pinpoint ovulation: Since increases in E2 are typically detectable a few days before LH surges, measuring E2 will give you more information to confirm that you are approaching peak fertility — when your chances of getting pregnant are higher.
There are lots of nuances to the different testing options that are out there — from how you collect urine to how LH is quantified to how you read the results. Let’s break it all down for you.
Collecting the results
While some people feel more comfortable with strip-based ovulation tests, others feel more comfortable with midstream ones. There are some pros and cons to each.

The Modern Fertility Ovulation Test is a strip-based test.
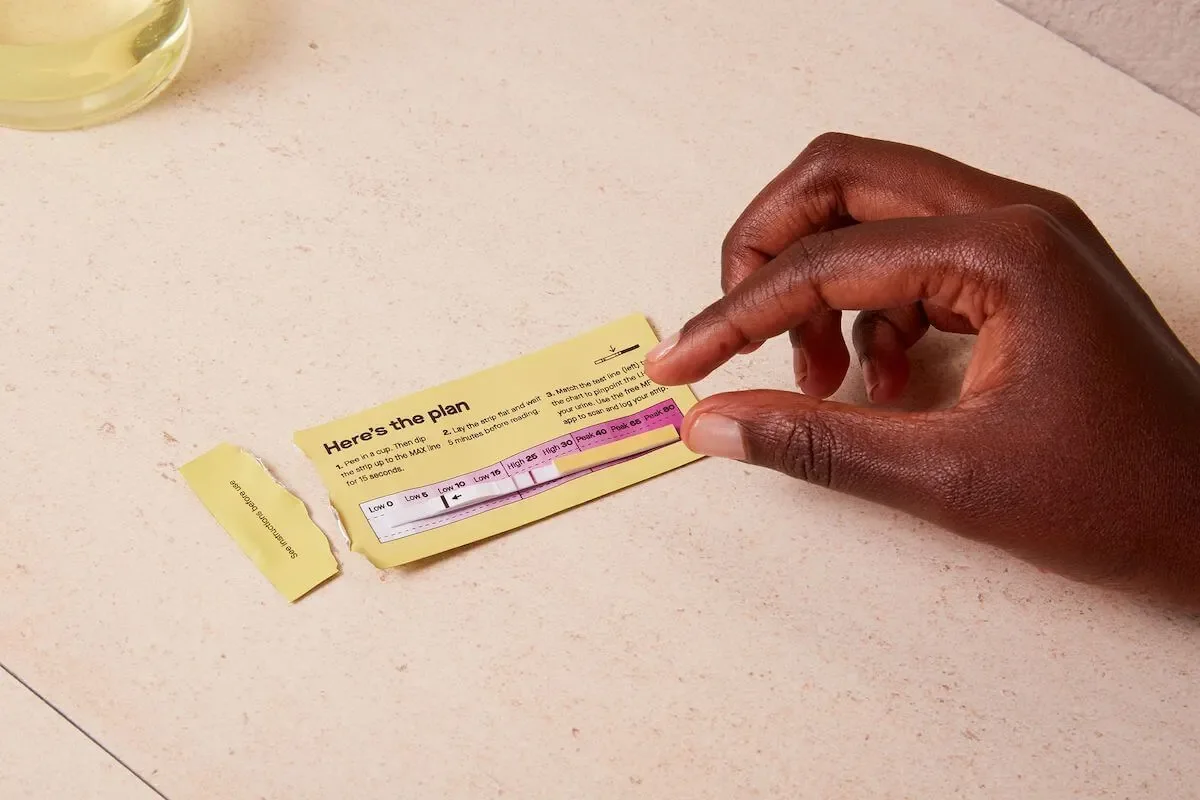
Strip-based tests (like the Modern Fertility Ovulation Test): Ovulation test strips are dipped into a cup of urine for approximately five seconds. With strip-based tests, you have total control over how much of the strip is exposed to urine, and for how long. (If the idea of peeing on a stick doesn’t thrill you, this might be the right option for you.)
Midstream tests: Midstream tests use the same strips used in strip-based tests, but surround them with plastic to help you position the strip while you’re urinating. If you prefer the packaging for midstream and the ability to cover the strip while waiting for the result, this could be the option for you. Keep in mind: Because more material is used to make midstream tests, they’re slightly more expensive than their strip-based counterparts.
Quantifying the results
Tests differ in terms of how LH is quantified. The ways LH is quantified in ovulation tests fall into two major classes — and these tests can be either strip-based or midstream. (Hooray for choices!)
Threshold-based tests: These tell you whether your LH surpasses a certain predetermined threshold that’s presumably indicative of ovulation — commonly, the threshold used is 25 mIU/mL or 40 mIU/mL (mIU/mL is milli-international units per milliliter). If the LH in your urine exceeds this cutoff, you’ll either see two equally-as-dark double lines, a “+” mark, a smiley face, or some other indicator that ovulation is likely near.
The Modern Fertility Ovulation Test is semi-quantitative to give you more insight into your LH levels.
Semi-quantitative tests: Instead of telling you whether you’ve surpassed a certain threshold, semi-quantitative tests, like the Modern Fertility Ovulation Test, tell you where your LH falls within certain ranges, such as low, high, and peak. They can give you a better idea of how your LH is changing over time, help you understand LH patterns, and can pinpoint your most fertile days.How to decide what’s right for you: Threshold-based ovulation tests work for people whose LH concentrations exceed 25 or 40 mIU/mL before ovulation. This may work for the general population, but often doesn’t end up working for many individuals (we call this “tragedy of the means”). For those with lower or higher baseline hormone production (like people with hypothalamic amenorrhea or PCOS), there may be inaccurate readouts. Our pick is semi-quantitative tests because they give you more detailed information about your hormone levels and get around some of the limitations of threshold-based tests.
That brings us back to the Modern Fertility Ovulation Test. We designed our semi-quantitative test to track your unique LH. Your test line will darken according to the levels of LH in your pee – so at a glance, you’ll know if your result is above the average LH surge threshold of 25mIU/ml when the test line is darker than the control line on the strip. Then, your result then matches to low, high, or peak levels on the test pouch to map a unique LH curve.
Interpreting the results
You can decide if you want an analog or digital readout of the results. Analog: With analog ovulation tests, it’s up to the user to decode what the test’s readout is. For threshold-based analog ovulation tests, you’ll see two lines — one dark line (the “control” line) should appear to indicate that the test is working, and a second dark line should appear if your LH exceeds the predetermined threshold, suggesting that you’ll release an egg soon. A line that’s lighter than the control line means your LH is below the threshold. This does mean the user has to do some interpreting — which can sometimes be hard to do accurately.Digital: For users who would rather have the results of tests interpreted for them and avoid misinterpretation, there are digital readouts, also sometimes called ovulation monitors. Instead of having lines of different color intensities used for readouts, digital readouts interpret your strips and tell you whether or not your sample reached the LH threshold by displaying a “+” or “-,” a :) or :(, or some other indicators. But this convenience and technology comes at a cost: Digital tests are more expensive than analog tests. And while using digital tests does take the guesswork out of interpreting an ovulation test result, this technology can sometimes be faulty — some digital tests have even been pulled off the market.
How to decide what’s right for you: How comfortable you feel interpreting test strips and how much money you want to spend will ultimately dictate whether an analog or digital ovulation test is right for you. The Modern Fertility Ovulation Test is analog to increase accuracy and save you on costs. We also include a handy color chart with your test to make interpreting your results super easy.
When should you use ovulation tests?
The exact guidelines for how you should use ovulation tests depend on how regular and long your cycles are. The “textbook” 28-day cycle sees ovulation occurring on day 14. In these cases, ovulation test manufacturers recommend starting to test a couple of days before the anticipated day of ovulation.
Chances are, though, that you don’t have a “textbook” cycle — simply because most people don’t. Cycles are commonly shorter or longer than 28 days, and it isn’t always the case that ovulation happens exactly in the middle of the cycle. If this sounds like you, the conservative approach would be to start testing a couple of days after your period ends and to continue testing until you get indications that ovulation is coming up. For example, for our Ovulation Test, we recommend you start testing 19 days before the start of your period. To figure out when that is, you’ll need to determine your cycle length and subtract 19 days from that number.
Regardless of when in your cycle you start using ovulation tests and which type of test you use, the way you use them should be similar and consistent. Because LH peaks are very transient (though again, this applies to the “textbook” pattern of cycle-based hormonal changes), ovulation test manufacturers often recommend testing once every 12 hours around the time of anticipated ovulation to make sure that the peak isn’t missed. They’ll also recommend that you test at approximately the same time of day each day and that you avoid testing after drinking excessive fluids (because your urine will be too diluted).
Give me the numbers: How accurate are ovulation tests?
Detecting LH and predicting ovulation
Though ovulation tests are likely better than the other cycle-tracking measures, you might be wondering: How good are they? Luckily, manufacturers of many tests will provide numbers on two key metrics — positive predictive value (the percent of people who are ovulating when the ovulation tests tells them they are) and negative predictive value (the percent of people who are not ovulating when the ovulation tests tells them they are not) — to give us an idea of how accurate a test is.
Though ovulation tests are likely better than the other cycle-tracking measures, you might be wondering: How good are they? Luckily, manufacturers of many tests will provide numbers on two key metrics — positive predictive value (the percent of people who *are* ovulating when the ovulation tests tells them they are) and negative predictive value (the percent of people who are *not* ovulating when the ovulation tests tells them they are not) — to give us an idea of how accurate a test is. Here’s what we know:
Pros: Know when you’re
According to test manufacturers, the negative predictive value of ovulation tests is excellent.
If an ovulation test indicates you are not having an LH surge, there’s around a 98% chance you are not going to ovulate in the next 24-72 hours and you’ll know that your chances of getting pregnant are not as high.
Recent data from a multi-center academic study confirms this: Regardless of what LH threshold was used to classify a “positive” LH surge, levels below the given threshold (so a “negative” test result) meant that ovulation did not happen within 24-72 hours for 98% of cycles examined.
Cons: Risk of false positives.
However, the opposite isn’t true — if a threshold-based test indicates you are having an LH surge, there’s a chance you’re not going to ovulate within the next few days.
Data from the same multi-center study found that using a threshold of 40 mIU/mL of LH in urine, only 23% of women with a detected LH surge ovulated within 24-72 hours.
Using a threshold of 25 mIU/mL, this number was closer to 50%.
Here’s another way of putting it: Among women who got a positive ovulation test, 50% to 77% of them didn’t actually ovulate within 24-72 hours of getting that positive test result.
There are ways to increase the positive predictive value of ovulation tests, though. For example, when considering both LH surges and cervical mucus characteristics together, the positive predictive value can increase.
The accuracy of threshold-based tests will also depend on what your average LH levels look like. There is a lot of natural variation in LH production across the cycle but also among different women — while some women may have LH levels around 4 mIU/mL two days before ovulation, other women have LH levels around 48 mIU/mL. Similarly, women on the lower end of LH production may have LH peaks at 24 mIU/mL, while this number is closer to 112 mIU/mL for women on the higher end of LH production.
The take-home here? False positives can be expected for women on the higher end of LH production, and false negatives can be expected for women on the lower end of LH production.These numbers come from ovulation tests that use threshold-based detection methods, but it’s likely that these percentages would be different when considering semi-quantitative tests. Some industry-sponsored studies of digital, semi-quantitative tests have found that “peak fertility” was detected by the test in 91% of cycles in which ovulation occurred. And that in 91% of cycles, ovulation occurred during the days classified as “peak fertility” days. Because the analog versions of semi-quantitative tests are newer than the digital versions, we don’t have reliable data on their accuracy yet.
Readability of the results
As we were developing the Modern Fertility Ovulation Test, we found plenty of the manufacturer studies we mentioned earlier about the accuracy of the tests themselves — but we were surprised to see a lack of published studies on how accurately people were able to actually read the tests’ results. (Because if a highly accurate ovulation test can’t easily be read and interpreted, we’re missing a big piece of the testing puzzle.)

Negative, Positive, and Invalid Ovulation Test Strip Results
Can medications impact the accuracy of your ovulation test results?
Hormones found in birth control medications — particularly estrogen and progesterone — can decrease your LH levels and affect your results. Drugs containing testosterone also decrease LH levels and can affect your results.
One of the fertility drugs used in fertility treatment, clomiphene citrate (Clomid), increases your LH levels to help you ovulate, and will affect your results.
How much do ovulation tests cost?
Prices vary depending on the brand and quantity of strips, but typically range from $15-$50, with strips for digital readers being more expensive. Here at Modern Fertility, our test strips are fairly priced so as many people as possible can get access to this important information.
You may also be able to get the cost of test strips reimbursed if you have a health savings account (HSA) or flexible spending account (FSA) as part of your health insurance plan.

Cervical mucus tracking
How do ovulation tests compare to other cycle-tracking measures?
There are so many reasons why you might choose to use one cycle-tracking measure over another. Your best option might depend on what your goals are (i.e., if you’re chasing conception or running away from it), how much money you want to spend, and how much self-education you want to do, among other things.
Here are a few other frequently used methods of ovulation tracking out there:
Cervical mucus will change in its consistency prior to ovulation, and these changes are directly driven by cyclic changes in estradiol (E2) production. Because E2 peaks a few days before ovulation, the cervical mucus will have distinct characteristics that signal to you that ovulating is coming up.
In contrast, basal body temperature rises after ovulation, so monitoring your basal body temperature across your cycle can tell you once ovulation has already happened (and if it happened at all), making it great for people who want to avoid conception. That being said, body temperature is affected by a whole host of factors, making body temperature alone not a super accurate marker of cycle phase.
Tracking progesterone: Because significant rises in progesterone are only seen when ovulation happened, progesterone can tell whether you’ve ovulated in the recent past. But, it doesn’t give us any clues about whether you’ll ovulate in the near future, or whether you’re ovulating right now.
Counting-based methods that rely on information about your cycle lengths alone to predict when ovulation will occur fall toward the bottom of the list as far as accuracy goes. This is because there’s so much variability in how long cycles are and when during the cycle ovulation occurs that just knowing information about the day of the cycle during one cycle doesn’t tell you all that much. Some cycle-tracking apps will use counting-based methods in conjunction with user-input characteristics, such as cervical mucus consistency or LH strip readouts, which increase their predictive accuracy.
For most of these methods, there are clear trade-offs in convenience and accuracy. Of frequently used methods, counting-based methods are the most convenient and require the least amount of effort, but are likely the least accurate. Cervical mucus monitoring takes more time and effort, but is more accurate in pinpointing the fertile window.
Generally speaking, the most accurate cycle-tracking measures will be the ones that measure ovulation most directly. The most direct measure of ovulation is an ultrasound — where doctors can actually visualize whether there’s an egg that’s been released from the ovaries.
For those of us that don’t have an ultrasound machine and ultrasound technician in-house (i.e., all of us), the second most direct measures are the hormones that are biologically implicated in predicting ovulation (like LH and E2).
The third most direct measures are things like cervical mucus and basal body temperature, which are associated with the hormones that are associated with ovulation. Each step removed from ovulation itself makes things more complex to interpret, and potentially introduces error — both of which affect how accurate a measure is.
Bottom line: Do ovulation tests work?
Ovulation tests get a big thumbs-up from us. They involve the measurement of reproductive hormones (which we’re big fans of here at Modern Fertility) and thus use relatively direct biological indicators of ovulation to help you figure out where in your cycle you are.
Because we’re hormone nerds — and proud of it — we offer a few different ways to measure and understand the hormones most important to fertility. First, the Modern Fertility Ovulation Test tracks your LH at low, high, and peak levels to help you predict ovulation and your fertile window. If you’re trying to conceive, the Modern Fertility Pregnancy Test lets you test for pregnancy and trust the result. Finally, you can use the Modern Fertility Hormone Test to understand how your fertility is changing over time. Our hormone test gives you insight into the number of eggs you have and can help you identify red flag issues — like PCOS or thyroid conditions — that could affect your reproductive health down the line.
This article was written by Talia Shirazi, and reviewed by
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.










