The ins and outs of the IUD: IUD side effects, effectiveness, and cost

Reviewed by Eva Marie Luo, MD, MBA, FACOG,
Written by Chanel Dubofsky
last updated: Dec 09, 2021
9 min read
Here's what we'll cover
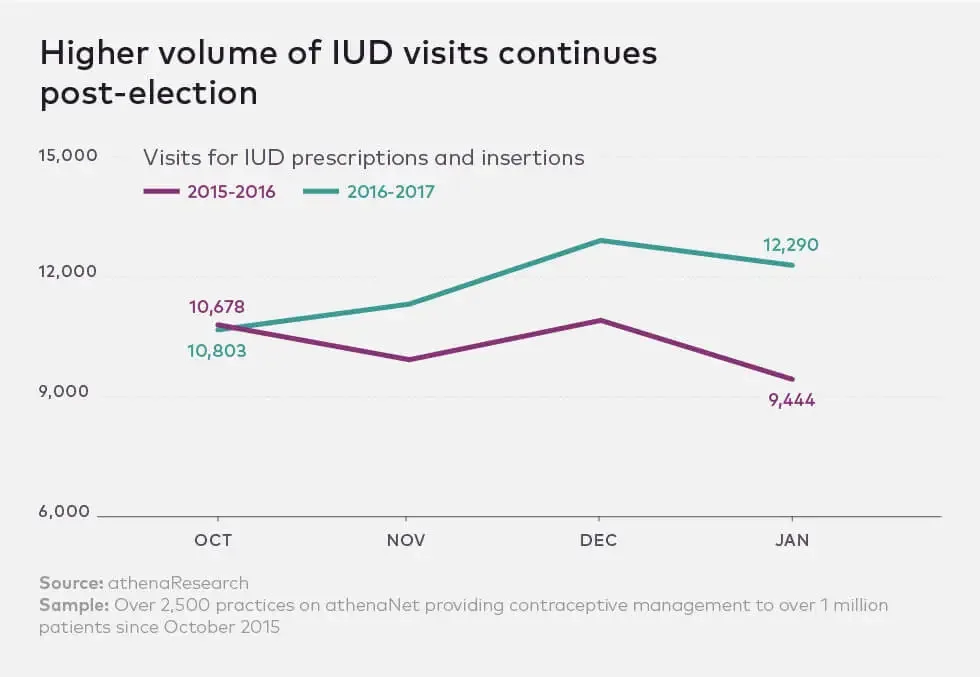
Intrauterine devices, or IUDs, are not new birth control options — but their popularity is rising. 8% of women ages 15-49 in the United States choose IUDs to keep watch over their uteruses. And in the last few years, there’s been a rather, well, interesting spike in IUD use. According to both Athena Insight and Planned Parenthood, IUD demand has increased exponentially since November 2016.
Hmm... wonder why.
Many say that IUDs are the most effective form of birth control on the market today — and study after study deems them safe for women of all childbearing ages. A 2015 study even showed that women’s healthcare providers use IUDs more than any other form of contraception. (We’ll have what they’re having!)
So let's get into it! In this piece, you'll find out:
How IUDs work
The differences between hormonal and non-hormonal IUDs
The pros and cons of the IUD
How to know if an IUD is right for you
What it's like to get and have an IUD (from real people!)
How does the IUD work?
The IUD is a small T-shaped device (adorable, really) that takes about five minutes to place inside your uterus. There are two types of IUDs: hormonal and copper (non-hormonal). And FYI: Conception is defined as a fertilized egg implanting in the uterine wall. So, the abortion fear of IUDs isn’t an issue because conception never actually occurs.
How the hormonal IUD prevents pregnancy: sperm shall not pass
Mirena, Skyla, Liletta, and Kyleena are not just excellent names for your new puppy — they’re the four brands of hormonal IUDs currently available. (Also, please let us know if you name your dog after an IUD — because that would be awesome.)
Hormonal IUDs prevent pregnancy by releasing the progestin levonorgestrel (LNG) and:
Thickening your cervical mucus so the sperm can’t reach the egg.
Making your uterus a hostile environment for sperm and eggs, impairing any chance of implantation by inhibiting the sperm’s ability to swim toward the egg.
Thinning out the inner lining of the uterus, impairing implantation and also giving you lighter periods (or sometimes no period at all).
Hormonal IUDS can interrupt your cycles, but most women won't experience any changes to ovulation. Studies show that in the first year, about 45% of cycles were ovulatory for women using Mirena, 45-75% for women using Liletta, 88% for women using Kyleena, and 97% for women using Skyla (the latter two are both lower doses).
The differences between these three brands are:
The amount of hormone released: Skyla, for example, releases 19.5 micrograms/day of progestin while Mirena releases 52.
The size: Skyla and Kyleena are slightly smaller and have a narrower inserter, so insertion may be a bit more comfortable — which is all kinds of good.
The approved length of use: Liletta is effective for up to six years, Mirena and Kyleena for up to five, and Skyla for up to three. However, there are promising studies (here and here) looking into the effectiveness of Mirena and Liletta for up to seven years.
How the copper IUD prevents pregnancy: not a sperm favorite
The other IUD option is the copper IUD (brand name: Paragard). The copper IUD prevents pregnancy by releasing copper ions into your cervix — no hormones here. Copper makes your uterus a pretty hostile environment for sperm for up to 10 years.
And on top of all that, copper actually, um… decapitates sperm. So, yeah, no fertilization.
The upsides, the downsides, and the good-to-knows
Now that you know the different types of IUDs and how they work, let’s talk through everything from side effects to costs, so you can make the most informed decision for yourself.
What are the advantages of an IUD? Here's why they've been increasing in popularity:
IUDs work. They're 99% effective. Studies have even shown that the IUD is comparable to female sterilization (which is crazy) with cumulative pregnancy rates at five years of <0.5%. Plus, copper IUDs can even act as emergency contraception up to five days after unprotected sex.
They're long-acting. Your IUD can stay in your body for 3-10 years, depending on the type you get. Think set it and forget it — crockpot style.
They’re reversible. Once you decide you’re ready for something new, you can have it removed and you should be able to return to your normal cycle right away.
They don’t mess with estrogen, which means fewer side effects than the pill. Hormonal IUDs release a localized hormone (the synthetic hormone progestin) and copper IUDs don’t contain hormones at all. More on that later.
They’re , meaning that IUDs can be placed immediately after delivery.
They won’t be (if inserted properly).
They’re sometimes free (at least for now). In May 2015, the Obama administration stated that under the Affordable Care Act, at least one form of all 18 FDA-approved methods of birth control, including the IUD, must be covered without a co-payment — even if you haven’t met your deductible. We’re hoping that, despite some recent developments, it stays that way.
You may be wondering why IUDs haven’t always been a fan favorite. There was a big controversy — call it the IUD version of “Serial” — in the ‘80s that gave them a pretty bad rep. It all had to do with the release of the Dalkon Shield, a faulty IUD that let bacteria into the uterus causing inflammation, infection, and infertility. Not good.
The incident ruined the USA’s trust in IUDs for years to come. Meanwhile, the rest of the world charged ahead. China, France, and Scandinavia kept on using their safe and effective IUDs (fun fact: 25% of Scandinavian women rely on IUDs!).
We now have nearly 30 years of science to back up the fact that IUDs are safe and effective. Now, that doesn’t mean there aren’t risks (we’ll get into those a bit later), but all IUDs recommended by doctors today are FDA-approved.
What are the side effects of IUDs?
Although IUDs are perfectly safe and effective, they’re not a magical, risk-free answer to birth control (even if they might seem that way) — they do have listed side effects. These side effects are primarily related to their effects on your monthly bleeding pattern.
Paragard copper IUDs can cause heavier and crampier periods. And for some patients, this can lead to anemia. Other listed side effects include:
Backaches
Bleeding between periods
The most common include:
Irregular periods
Lighter or absent periods — but this will typically go away within a few months.
Mild bloating
Mood changes
Cramping or pelvic pain (if experienced immediately after insertion, that will resolve — if experienced later, it may be a sign that the IUD was not inserted properly or has migrated)
Skyla's include:
Irregular or missed periods
Spotting or bleeding between periods
Mild bloating
Cramping or pelvic pain
Both the hormonal and non-hormonal forms of IUD come with the risk of accidental “perforation,” or, well, a hole in the uterus and “expulsion” of the IUD. Expulsion, you ask? Yeah. There is a small chance that the IUD can slip out of your uterus. Planned Parenthood assures us that this is very rare (occurring between 2 and 10% of women), and usually due to improper insertion.
According to the
You've previously expelled an IUD
You've never been pregnant
Your periods are heavy and prolonged
You have fibroids (benign tumor-like growths of the uterus)
You have severe menstrual pain
You're younger than age 25
Your IUD was inserted immediately after childbirth
Doctors do a check of the IUD’s strings (there are little teenie strings on the bottom of the IUD for removal) about 2-3 months after insertion to make sure it’s in there nice and snug.
How can an IUD impact fertility?
As we've mentioned, an IUD is long-term birth control. So what happens when you get it removed? Can you get pregnant right away?
When you stop taking hormonal birth control, there are side effects, which vary from person to person, as your body returns to its pre-BC state. However, when it comes to your post-IUD fertility, a 2011 report that reviewed the literature about hormonal IUDs confirmed that "normal fertility is regained after a few months, with a near-normal 80% of women able to conceive within 12 months.”
According to a 2015 study of 69 former IUD users (50 copper and 19 hormonal) and 42 former non-IUD users, there was no difference in the time to pregnancy in IUD users compared to non-IUD users. Black women did demonstrate a significant statistical difference in terms of fertility, however, which authors plan to address in a larger study.
Depending on what kind of IUD you use, you might be able to get pregnant immediately after your IUD is removed. If you don't want to conceive right away, it's a good idea to avoid vaginal sex at least seven days before you get your IUD removed, depending on when you ovulate, and to use another form of birth control if you do have sex.
Here's what does have the potential to adversely impact your fertility:
Leaving your IUD in past its removal date. An expired IUD isn't an effective form of birth control. Whether you are trying to get pregnant or avoid pregnancy, remove the IUD when it expires. If the IUD is left beyond its removal date, this can possibly, but rarely, lead to an infection, which, if left untreated, can lead to infertility.
If pregnancy does occur while you're using any IUD (remember, it’s super rare, less than 1% of patients using an IUD will get pregnant), there's a risk of ectopic pregnancy, which is when the fetus develops outside of the uterus. An ectopic pregnancy is not viable and is also extremely dangerous. One treatment for ectopic pregnancy is the removal of a fallopian tube, which can impact your fertility.
When you're getting your IUD removed, it's important to note that you may experience some slight cramping during and right after removal. Severe bleeding is rare, so talk to your doctor if you're bleeding heavily after IUD removal.
How much does an IUD cost (and will insurance cover it)?
Without insurance, an IUD alone can cost between $500 and $1,000, but if you do have insurance, an IUD can be super low cost — or even free. The Affordable Care Act mandates that birth control, including the IUD, is covered by insurance plans, but you should check in with your provider to be sure. Planned Parenthood also offers programs that make getting birth control, including IUDs, affordable for folks without insurance.
Keep in mind, though, that the total cost of your IUD involves more than just the actual device. You should factor in:
What kind of IUD you're getting (cost varies according to brand)
The co-pay for your initial GYN exam
Getting your IUD inserted (more on this later)
The co-pays for your follow-up visits
While the cost of an IUD without insurance is more expensive than other birth control methods like the pill, remember that it's long-term birth control, so once it's in, you've got as many as 10 years (depending on what kind of IUD you have) before you need to think about spending that money again. In fact, one study even suggests that it’s one of the most cost-effective contraceptive options we have.
To IUD or not to IUD?
Despite the warnings, studies have deemed both IUD types as “highly acceptable with few unanticipated side effects.” And although the copper IUD is slightly more effective (with pregnancy rates between 0.3% and 0.6%), the hormonal IUD is only slightly less effective (<0.5%).
So, which to choose? Talk to your doctor and they'll walk you through the options. They’ll make sure you’re a great candidate by:
Ensuring you’re not already pregnant and don’t have any infections
Asking you about your sexual history
Checking the position of your uterus
Discussing your current monthly bleeding patterns
Your fertility goals
If you want to avoid hormones, a doctor may suggest you choose copper or, since the hormones are localized and don’t have as broad of an impact as the pill, they may still recommend a hormonal IUD. If you have heavy bleeding, a doctor may suggest you avoid Paragard, which can make things really flow.
Who should and shouldn’t get IUDs
IUDs are a great birth control option for many women, but, according to Planned Parenthood, you may not be a good candidate for an IUD if you:
Currently have an sexually transmitted infection (STI) (once treated, this can be revisited)
Have a pelvic infection
Think you're already pregnant
Have untreated cervical cancer or uterine cancer
Have any clot-preventing blood disorders
Have had breast cancer
And you should avoid the non-hormonal Paragard IUD if you:
Are allergic to copper (the non-hormonal kind is made from copper)
Have Wilson’s Disease (in which high amounts of copper accumulate in the body)
In some rare cases, uterine size or shape could make it difficult to insert an IUD. But, like we mentioned earlier, your doctor will walk you through whether or not the IUD will work for you — and there are plenty of other choices if it won’t!
If your doctor does deem IUDs as appropriate for you, there’s a huge perk for anyone suffering from PMDD, or premenstrual dysphoric disorder — studies show that IUDs, among other forms of contraception, may be very helpful in treating the symptoms.
How is the IUD inserted?
Your gynecologist “installs” (not the medical term, but that’s definitely what it feels like) the IUD into your uterus using a small insertion device. There is speculum action. There is cramping action. There is spotting. It’s not I-need-to-lie-in-my-bed-right-now cramping, but almost. And how to describe the feeling? It’s not a tampon in your vagina feeling — it’s an “oh… oh okay, that’s different,” kind of feeling.
Overall, it’s not excruciating — but it’s not comfortable. Your doctor may recommend taking an ibuprofen or two one hour before your appointment. And then you’ll go about your life (and sex life), enjoying the perks of sexual empowerment knowing you’re locked and loaded with safe, effective contraception. Check in with your doctor monthly to make sure everything’s working as it should!
What's it like to get and have an IUD?
Christine calls her Mirena IUD “a godsend.” She needed a birth control method that made “less of an impact” on her hormones, and “as someone who is massively impacted by hormones, it’s been a breeze. Not getting a period is the best.”
Sarah had similar feelings: “My periods are light to non-existent. I never have to think about taking a pill. I haven’t experienced any weight gain or heightened emotions. I feel steadier than ever, as if PMS has been mitigated.”
And for some women, like Kate, the IUD just straight up wasn't right. Kate says, “My copper IUD made me bloated and gave me a heavier period than ever. I had it removed a few months in. I may try a hormonal one down the road, but I’m not sure it’s the right thing for my body."
Okay, one last thing
Remember, remember, remember that IUDs protect against pregnancy, but not in the slightest against STIs. If you and your partner haven’t been tested for all of the things, keep the condoms handy. We’re here to arm you with info, but only your doctor can give you medical advice. If you're thinking through BC options, talk to them first.
This article was medically reviewed by Dr. Eva Marie Luo, an OB-GYN at Beth Israel Deaconess Medical Center and a Health Policy and Management Fellow at Harvard Medical Faculty Physicians, the physicians organization affiliated with the Beth Israel-Lahey Health System.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.










