Free shipping
FSA/HSA reimbursable
These customers received compensation in exchange for their testimonials.
Hear it from our customers
Becca Kufrin
"I’ve been using Modern Fertility's Hormone Test since 2020 to help me better understand my body and where I’m at fertility-wise based upon my age and lifestyle."
Briana Myles
"Modern Fertility is the G.O.A.T when it comes to Fertility testing and tracking! Their method is low cost, fast, and effective. My results came back in just 10 days. "
Caroline Lunny
"I was 29. Regular periods, no symptoms, no reason to be concerned. Because of Modern Fertility, I found out that something was silently wrong for years. MF gave me a ground to stand on when I had to stand up to doctors who said I was too young to have hormone levels that low."
Shawn Johnson
"Modern Fertility gives you insight into your ovarian reserve, thyroid health, and other hormone factors. You can take it from home and your results come in an easy-to-understand dashboard."
The same hormone test typically offered by reproductive endocrinologists for a fraction of the price. We'll test between two and seven hormones based on your birth control method, and deliver custom reports to help you learn about your fertility.
Customized for your birth control
Reports created with fertility doctors
Connect with a fertility nurse
Invite to the Modern Community


Accurate
The same fertility hormone test typically offered in clinics. Validated with a clinical study. All results are based on clinical thresholds set by fertility doctors.
Affordable
A fraction of the cost of fertility clinics.
Easy
Simple, at-home finger prick kit (you can even do it in your PJ’s!). Then just mail it back to our lab.
Supportive
The Modern Community makes it easy to connect and get questions answered by a fertility nurse.
Testing 101
01
Order your test
We’ll customize it based on your birth control. You can collect your sample at home or at a local Quest Diagnostics lab.
02
Collect & mail your sample
Complete your simple finger prick, then pop your sample in the mail and send it to our lab.
03
Receive your results
Once your sample arrives at the lab, you’ll get your results in about 3 business days. We’ll benchmark your results against the clinical guidelines set by fertility doctors.


Backed by top physicians
“Information garnered from a fertility hormone panel can help people understand how their fertility changes over time so that they can take action and be proactive about their fertility planning.”
– Dr. Jenn Conti, MD, MS, MSc. OB-GYN and medical advisor for Modern Fertility
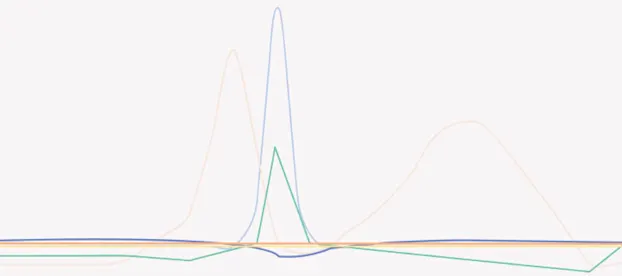
Which hormones will I test?
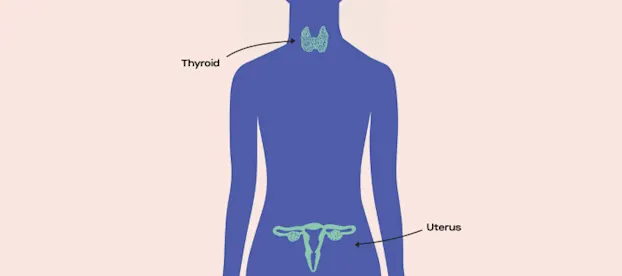
We customize your test based on whether or not you’re using hormonal birth control. If you’re on hormonal birth control, you can get an accurate read of your AMH and TSH levels to learn more about ovarian reserve and thyroid health.
Anti-Mullerian Hormone
AMH is released by cells around your follicles and is the most important hormone for testing ovarian reserve (the eggs you have “waiting in the wings”).
You'll test AMH even on birth control.
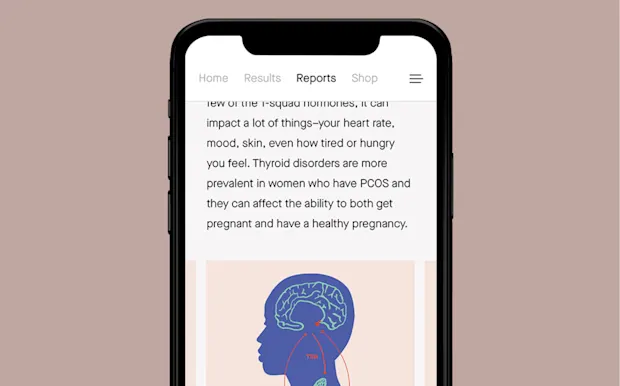
Thyroid-Stimulating Hormone
Produced by your pituitary gland, TSH regulates thyroid health.
You can test TSH even on birth control.
Follicle-Stimulating Hormone
Responsible for growing follicles and starting ovulation. Too much FSH can mean your body needs extra oomph to get things moving.
You’ll test FSH if you’re not on hormonal birth control.
Estradiol
A sex hormone produced by the ovaries. Since high E2 can mask a high FSH, we test these hormones together.
You’ll test E2 if you’re not on hormonal birth control.
Free Thyroxine
fT4 plays a role in thyroid health, especially when tested with TSH. If you have certain TSH levels and are not on hormonal birth control, we’ll send you another kit to test your fT4.
Prolactin
Stimulates milk production and pauses ovulation after you give birth.
You’ll test PRL if you’re not on hormonal birth control.
Luteinizing Hormone
Produced by your pituitary gland, LH regulates the length of your cycle.
You’ll test LH if you’re not on hormonal birth control.
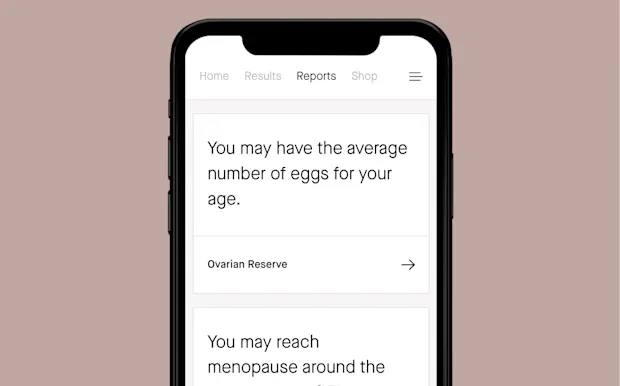
What will I learn?
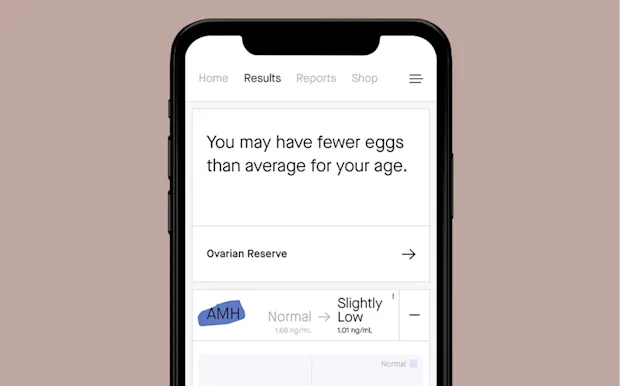
01
All about your eggs, aka your “ovarian reserve”— if you have more or fewer eggs than average for your age.
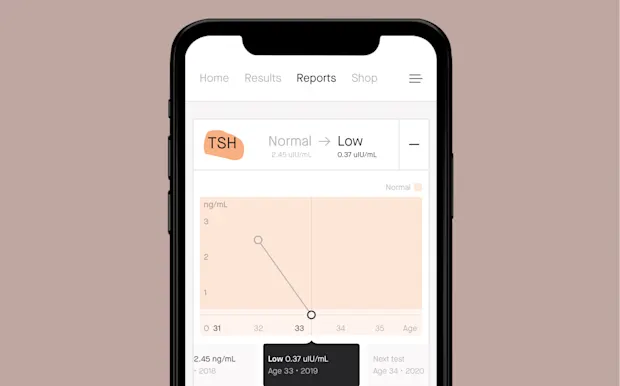
02
Your thyroid levels. Thyroid can affect your mood, skin, weight, energy, and ovulation.
03
If you have any fertility red flags so you can have personalized conversations with your doctor.
04
About your AMH levels, which doctors can use to get signals about if you could hit menopause earlier or later than average.
05
If a doctor might expect to retrieve more or fewer eggs than average for egg freezing or IVF.

See a sample fertility hormone test report


Our in-depth results walk you through your hormone levels and what they mean for your fertility goals and overall health.
Patient Reviews
4.5 (2216 reviews)
3/24/2023
Melissa
Informative
Very easy to send in samples. There was a glitch in the system, so they never received my lab results. I had to contact the company and they were able to resend the lab results and I received my detailed results a few days later. Overall I am happy with the information received.
3/24/2023
Melissa
3/19/2023
Amanda
I expected more information from
I expected more information from the test results for the price. But it’s a good start.
3/19/2023
Amanda
3/17/2023
Christina
I only wish I had done this sooner!
I just got the results from my third time testing with Modern Fertility in the past 2.5 years. I’m so glad I went with testing, and my only regret is not testing sooner! The entire process was very seamless and the home testing was simple. I appreciate the detailed dashboard with results- I’ve usually gotten my results within a few days of mailing my test back! While my results were a bit disheartening, I felt empowered to make an appt with my OBGYN and start discussing my options sooner. I ultimately feel more empowered with the information I have from my tests, and can make better decisions having this!
3/17/2023
Christina
Answers to your hormone test questions
The Modern Fertility Hormone Test is extremely accurate. Whether you collect your sample with our at-home collection kit or choose to go into a Quest lab, you’ll get accurate results from your fertility hormone test. We conducted a clinical study demonstrating that capillary blood collected with the Modern Fertility at home collection kit and a traditional blood draw can be used interchangeably to measure reproductive hormones.
This clinical study was published in the February 2019 edition of Obstetrics & Gynecology (the “Green Journal”), the Official Publication of the American College of Obstetricians and Gynecologists.
We’ll send you everything you need to test, along with instructions (and tips!) to support you throughout the process. After you collect your blood sample with a simple finger prick, you’ll just pop it in the mail and our lab will handle the rest.
It typically takes about 7 days to get results after your sample arrives at our lab. In total, expect about 10 days from the time you drop your sample in the mail. We’ll send you an email when your results are ready to go so you can login to your personalized fertility dashboard!
Testing on birth control can help you get proactive with fertility insights even before you’re ready for kids. If you’re on hormonal birth control you’ll test two key fertility hormones: AMH, the most reliable hormonal marker for ovarian reserve, and TSH, the main indicator of thyroid health. Each Modern Fertility Hormone Test is customized for you based on your birth control and the regularity of your period (if you get one).
In general, fertility testing is not covered by most insurance plans unless you’ve been actively trying to conceive for a certain period of time. Modern Fertility was founded after our CEO, Afton Vechery, spent $1,500 getting the same panel of tests through her doctor. With Modern Fertility, you’re able to test the same fertility hormones that you would in a clinic, for a fraction of the price.
We’re not able to accept insurance for the Modern Fertility Hormone Test, but you can get reimbursed through your HSA or FSA benefits. Once you receive your kit at home, activate it, then download your HSA/FSA receipt to submit it for reimbursement.
The Modern Fertility Hormone Test is available in all US states except New York and Rhode Island.
Unfortunately, the Modern Fertility Hormone Test is non-refundable and non-transferable. This means that a Hormone Test that you’ve ordered cannot be returned for a refund or be used by a different person. If you are looking to gift someone a Modern Fertility Hormone Test, we recommend you purchase one from our Amazon page.
Yes! Your test will arrive in discreet packaging from “Modern Health.”
We created Modern Fertility to bring the cost of testing down and to make customized fertility hormone information more accessible. Your test results are just one piece of this. With your Fertility Hormone Test, you’ll also gain access to:
A free customized fertility planning tool based on your goals and timeline
A community platform where you can get your Q’s answered by fertility experts and connect with people who get it
Recommended reading
Why "cycle day 3" is so important in the world of fertility hormone testing
The Modern guide to AMH: Everything you ever wanted to know about anti-Mullerian hormone
Keep shopping
More fertility essentials
Modern Fertility and Ro products are designed to give you more agency over your reproductive health, so you can own the decisions impacting your body and your future.
Modern Fertility Hormone Test
The most comprehensive fertility hormone test you can take at home to be proactive about your fertility.
Learn moreRo Sperm Kit
A trusted, easy, and fast way to test and store sperm.
Learn moreModern Fertility Ovulation Test
Find your 2 most fertile days, predict ovulation, and get in sync with your cycle.
Learn moreModern Fertility Pregnancy Test
Test if you’re pregnant and trust the result—plain and simple.
Learn moreModern Fertility Birth Control
Connect with a provider to get a prescription for the pill if it's appropriate.
Learn moreModern Fertility Prenatal Multivitamins
Developed with OB-GYNs to prep your body now for kids whenever.
Learn more